A short intro explaining the H1: quick definition of bone tooth loss, why it matters for chewing, appearance, and planning for dental implants. Bone tooth loss means the jawbone around a missing or failing tooth shrinks over time. This loss affects chewing, speech, and your smile. Left untreated, bone loss can make future dental implants harder or impossible without extra surgery. Early action preserves bone and keeps more implant options open.
What is bone tooth loss?
Bone tooth loss is the gradual shrinking of the jawbone where a tooth used to be. Teeth stimulate the bone when you chew; without that stimulus the bone “resorbs” or melts away. Less bone means less support for nearby teeth and less foundation for implants, so acting early helps improve implant success.
Common causes of bone tooth loss
Periodontal (gum) disease
Gum disease is an infection that destroys the tissues holding teeth and the underlying bone. If untreated, pockets form, bone recedes, and teeth loosen. Controlling gum disease early slows or stops bone tooth loss.
Missing teeth and natural resorption
When a tooth is removed and not replaced, the socket loses volume. Over months to years the ridge narrows. This natural resorption is a main reason dentists recommend prompt replacement to limit bone tooth loss.
Trauma, infection, and aging
Accidents, long-term untreated dental infections, and general age-related bone loss also reduce jaw height and width. These factors can speed bone tooth loss and limit implant choices.
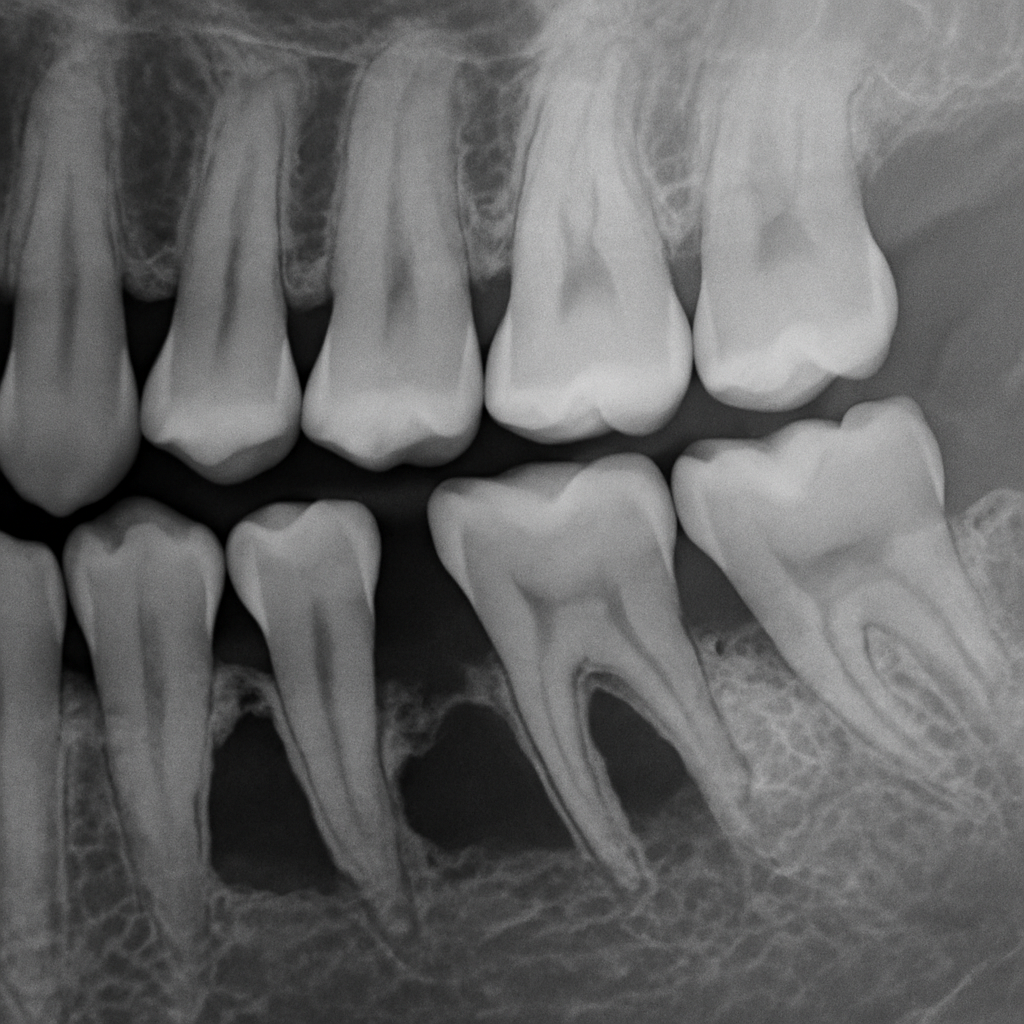
How bone tooth loss is diagnosed
Look for signs like loose teeth, shifting teeth, or receding gums. Imaging is key: digital X-rays show bone levels, but CT scanners and 3D digital scans give accurate views of bone volume and shape. These scans let your dentist plan implants precisely and spot areas needing grafts.
How bone tooth loss affects dental implant options
If bone is adequate, a simple implant and crown may work. Moderate loss often needs bone grafting or ridge augmentation before or during implant placement. Severe upper jaw loss may require sinus lifts. More procedures mean longer timelines, higher costs, and staged treatment, but they improve implant stability and long-term success.
Treatment and prevention: restoring bone for implants
Bone grafting and ridge preservation
Common grafts use autograft (your own bone), donor bone, or synthetic materials to rebuild the ridge. Socket preservation after extraction places graft material to limit resorption. These steps restore volume to support an implant later.
Soft-tissue lasers and improved healing
Lasers can make precise incisions, lower bleeding, and reduce swelling. They often speed healing and improve comfort after grafts or implant surgery, helping the bone and gums recover faster. Soft-tissue lasers can be a part of this advanced healing.
Everyday prevention
Prevent bone tooth loss with good oral hygiene, regular cleanings, treating gum disease, and replacing missing teeth promptly. Early care keeps more implant options available.
What to expect during implant treatment
Typical steps: consultation and 3D imaging, planning, grafting if needed, implant placement, healing (osseointegration), and final crown. Sedation choices range from conscious options to IV sedation. Many practices use digital workflows for faster lab work and clearer timelines.
Why choose a board-certified implant surgeon
Board-certified surgeons bring advanced training and experience treating bone tooth loss with complex grafting and implant techniques. Dr. Eric M. George, DMD, DABOI, DICOI, MAGD, is a board-certified implant surgeon with advanced technology like CT scanners, digital planning, soft-tissue lasers, sedation options, and 24-hour support to guide complex cases safely.
Next steps
Schedule a 3D imaging consultation to assess bone tooth loss and create a personalized implant plan. A scan will show whether you need grafting or can proceed to implant placement and give clear treatment options and timelines. Contact the office to set up an evaluation.